Integration, Interoperability, and the Future of Healthcare
Unlocking clinical data will drive improved patient outcomes.
If there’s ever been a time for ensuring providers have access to the most accurate, connected data, it’s now.
Yes, healthcare organizations have successfully moved from paper filing systems to electronic health records (EHRs). But now, more than ever, we need a complete view of the patient to safely deliver care and promote the health of the population. How do we get there? The industry seems to have come to a consensus on the answer: through interoperable systems.
It wasn’t long ago we were shifting from paper to digital. Our ambitions grew as healthcare reached for a complete view of the patient, no matter where the data resided. Despite many incentives, data sharing advanced slowly. So, the U.S. Congress got on it, with the 21st Century Cures Act and its open APIs “without special effort.” The White House and CMS created the Promoting Interoperability incentive program and the MyHealthEData Initiative. And standards organizations and collaborations continued to promote standards adoption and advocate their use.
Salesforce and MuleSoft are a critical part of this effort, working diligently to provide the systems that can help organizations create a 360-degree view of the patient and foster a healthcare system that can attend to patient needs in real time — especially during a crisis like the COVID-19 pandemic or emerging situations such as the monkeypox virus. Interoperability is the brass ring in achieving these goals.
Competitive, cost, and security pressures are pushing us harder than ever toward an interoperability model. We see this come to life in the spate of recent megadeals, including Intermountain Healthcare and SCL Health's merger to create a larger Intermountain Healthcare, Advocate Aurora and Atrium Health's 67 hospital merger to form Advocate health, and Amazon buying One Medical. When healthcare organizations come together, so do their systems, creating an opportunity to gain insight from rapid aggregation. This all can lead more quickly to new strategies, products, and services. It also can lead to an invaluable source of truth for patient data — all of which will improve trust between providers and patients, and, ultimately, healthcare outcomes.
The initial phase of going digital helped create the EHR system. Now we aim to go beyond EHR, toward API-enabled, interoperable systems. Technology has advanced so much in the past decade, and with that, our Salesforce toolkit is so much more robust, with blockchain, advanced analytics, and, of course, CRM. They are not, however, all neatly packaged in the EHR.
At Salesforce, we see so many factors speeding us toward interoperability: the rise of value-based care and regulatory disruption, the accelerated creation of industry data and services, the need for virtual care, as well as the need to access modern digital capabilities. It’s all exciting but it will take time before interoperability becomes routine and patients can reasonably expect a consumer experience that is as convenient as ordering dinner online.
In this guide, we explore the need for interoperability in our healthcare system, the roadblocks preventing it from thriving, the interim steps we need to take, and the role of integration to provide that consumer experience that ultimately helps patients be more informed on their own healthcare journeys and lead a healthier life. Then we introduce you to industry pioneers who are paving the way for truly connected healthcare.
Chapter 1: What Is Interoperability?
The U.S. healthcare system is a vast web of systems, applications, and data. The majority of hospitals and private practices have implemented an EHR of some kind, which is helpful, but most of these systems are completely separate, often from different EHR vendors that cannot talk to each other. This last of interoperability isn't just across separate healthcare organizations but can happen within the same health system as well with disparate systems that are locked in data silos. All this hampers care coordination and stands in the way of improving health. These shortcomings result from three challenges:
- Siloed patient data across clinical and nonclinical systems. This creates fragmented experiences and missed opportunities for preventative and total health. Yet, many IT decision makers are still at a loss on how to connect the data, despite recognizing the need to adopt interoperability in order to improve data quality and patient experiences. With this in mind, fewer than 40% of providers in the U.S. reported that they've managed to embrace interoperability to the point where they can perform it well enough to be able to share health data with other organizations.
- Legacy health IT proving incompatible with modern engagement technology. This delays efforts for digital transformation. In fact, 64% of IT leaders cite legacy infrastructure, processes, and tools as a top barrier to transformation.
- System connections that are driven by point needs for data. This results in a growing inventory of point-to-point integrations that are costly to maintain and don’t scale well enterprise wide. And with 75% of U.S. hospitals managing more than 10 EHRs, maintaining these connections becomes exponentially cumbersome.
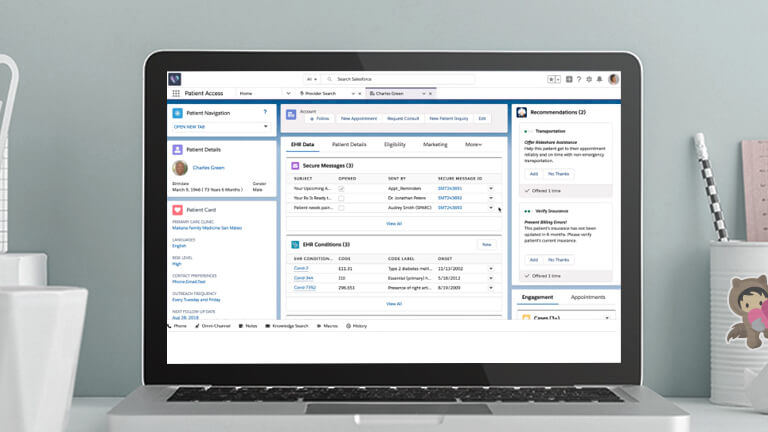
To truly achieve a complete view of the patient, healthcare organizations must be able to seamlessly connect with and act on data collected by the patients’ overall care team across multiple providers and do it in a secure way. And they must be able to preserve all the context that comes with the data. This is where interoperability shines.
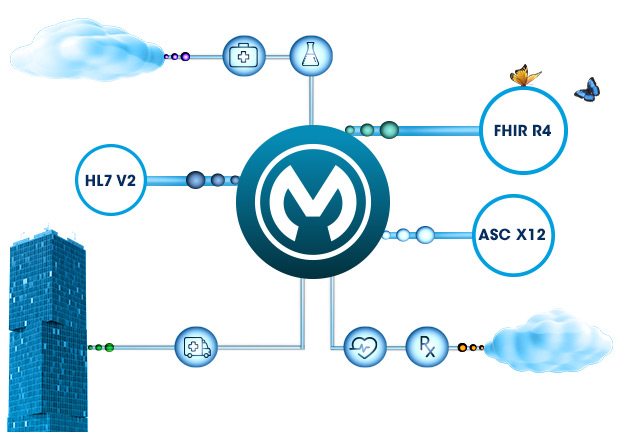
Interoperability takes systems integration to the next level. As it matures, interoperability can use integrated connections to drive meaning across systems by giving context to the data. It does this by enabling information systems, devices, and applications to access, exchange, integrate, and cooperatively use data in a coordinated way within and across organizational, regional, and national boundaries.
Integration connects disparate systems but may not carry the context of the information it brings together. It performs a vital function, orchestrating multiple interfaces that support process automation. It also brings together component subsystems into one system, ensuring that they function together as a unit. Integration is the foundation for interoperability.
While many systems integrate, the data they share frequently lacks context. By contrast, interoperable systems can talk to each other in the same language — preserving meaning, without the added complexity or delay. Interoperability allows computer systems to transmit data with increasing sophistication.
Interoperability is the ultimate goal. But healthcare won’t reach it until the entire healthcare IT ecosystem can seamlessly connect and transmit all clinical and nonclinical information necessary to drive the most well-informed, best possible outcome for each patient. Until then integration will continue to evolve to a higher level as it aims for meaningful interoperability.
Chapter 2: Salesforce’s Approach to Integrated Solutions
Discover how you can set up open, collaborative exchanges.
See how to:
- Create a patient-centric experience
- Unlock information across silos
- Find a solution that grows with you
- Define and understand use cases