Barwon Health
“It is a collaborative project, co-led by Clinical Informaticians, IT specialists, and subject matter experts to establish a new standard in connected, patient-centred care.”

Barwon Health is building a connected care platform that exemplifies analysts’ vision for the future.
We see a number of “customer-first” or “customer-centric” systems, but what Barwon Health is doing is truly impressive.
Barwon Health is one of Australia’s regional health services, providing primary care, emergency and acute care, aged care, community services, rehabilitation, and mental health to people at all stages of life. Its purpose or mission is to provide the best care to every person every day so that everyone feels better. “One day, I'm putting people back together who have injured themselves or found themselves in a situation of crisis requiring acute medical care. The next day, I'm making sure the patient has what they need to achieve the best care and improve their health before they have to come in and see me in the emergency department,” said Dr. Alastair MacKinlay, Medical Informatics Lead, Barwon Health. “One job compliments the other.”
So, it’s only natural that the systems Dr. MacKinlay is using to deliver this care are just as integrated. But as many healthcare professionals might tell you, integrated systems are more of an exception than the norm, which is what makes Barwon Health, the platform Dr. MacKinlay and team are building, and the strategy driving it such a noteworthy example for any public health or healthcare organisation.
Healthcare’s latest industry trends are a call to action.
Whether it's because healthcare providers spend decades developing very specific subject matter expertise, the way insurance tends to be stricter service by service, some combination of the two, or any other number of factors the reality is: healthcare tends to be a rather fragmented industry. And the industry was starting to show signs of disruption — as digital, integrated, self-service operations become more commonplace, they reset the expectations people have as a customer of any enterprise-level engagement — when COVID-19 hit and accelerated everything:
- At its 14th annual healthcare conference, McKinsey & Company found that virtual health visits grew by more than 3,000% during the pandemic for a total of 150 million telehealth claims in just two years, and that 60% of patients now expect to be able to change or schedule a healthcare appointment online. [1]
- As a result, PWC has started seeing a more empowered patient who exercises typical consumer behaviour even further. They are more open to healthcare at home, more open to telehealth for a wider variety of treatment programs, more open to retail vaccination clinics, more open to participating in clinical trials, and more vocal about topics like mental health. [2] Speaking of...
- Mental health, fitness monitors, wellness programs, etc. have become so popular that industry analysts are seeing them as an opportunity to deliver an unprecedented quality of care. “By integrating mental health offerings into existing physical health-focused organisations, such as primary care and inpatient hospital settings, attention to mental health can become more ingrained in the health care culture. Prevention and treatment protocols and plans can include whole-person health in lieu of solely focusing on physical health challenges, which never exist in isolation. There are no physical health problems without psychosocial components, and no psychosocial problems without physical health challenges. Integration can improve quality of care and satisfaction for consumers and providers, help to reduce mental health stigma, and reduce rates of avoidable health care spending,” reported Deloitte in its 2022 Global Healthcare Outlook study. [3]
“Very little of that data is connected today. All of it exists as individual appointment times with no one specifically there to coordinate because [the healthcare industry] has this paternalistic view of doctor or caregiver and patient,” said Bill Reynolds, Clinical Informatics Lead, Barwon Health. “But the more people you speak to in my space, the more you find people who want to change to that paradigm. They’re just unsure how.”
In other words, the pandemic demonstrated that industry transformation is possible, not detrimental, and what the Barwon team is doing now epitomises that.
Introducing Barwon's digital front door for patient care.
Barwon is building a community electronic medical record system (community EMR): a connected, patient-first, HL7-ready platform on the Salesforce Customer 360 Platform for Health. It gives clinicians the tools they need to enroll patients in programs as needed, connect that data and information accordingly, and give real-time visibility to care providers as needed so that everyone involved in the person’s care (including the patient!) can take action as one team.
Here’s how the EMR is designed:
- Authorised care providers log in to the portal via Health Cloud, Salesforce’s service and case management CRM product intelligently optimised for the needs of the typical patient interaction. Here, they can log notes in the patient’s personal profile record, tag clinicians or specialists on specific questions, update program enrollment details, and so on. “This will give staff the ability to stay updated on a patient without having to file through folder after folder of paper notes to find out the status is from program X, how successful program Y has been, what impact program Z has had...” said Reynolds.
- Integrated reports and dashboards pull patient data into a summary view, which staff can use to spot trends or patterns, measure relative progress, pinpoint catalysts, and more.
- Salesforce Field Service was added, which will extend the same functionality to Barwon’s extended network; hospitals or home nurses for example who make a significant number of house visits. These teams will also be able to log into the system, receive their schedule, look at a dashboard, determine who they need to visit next, and understand what that patient’s needs might be when they get there. I.e.: “a greater level of acuity across our hospital-in-home services, allowing more patients to recover in the comfort of their own house, faster,” Dr. MacKinlay added.
- Real-time and/or urgent updates can be sent to a care team via instant message through online community portals built using Experience Cloud. “Let’s say you’re one of our mental health workers and you have 15 active clients under your care, including Sandra who just finished a checkup appointment after testing positive for COVID-19 the week before. Sandra, or Sandra’s doctor, can log in and send you a message to let you know she’s struggling more today than yesterday, prompting you to follow up with her sooner than you might have otherwise and potentially stopping an acute crisis,” Dr. MacKinlay continued.
- MuleSoft was also included, enabling the system to integrate and automatically share records back and forth with third-party systems. As was Shield, giving Barwon the tools to build an additional layer of security and compliance features like event monitoring and field audit trail. And last but not least, Sandbox was layered on, providing Barwon with a test environment to try out new capabilities before pushing them live to the broader network.
Instead of having program-by-program progress reports that list patient names and outcomes one line after the next, everything starts with the individual and the care they are receiving. “We can incorporate and connect things like outpatient rehab, allied health, occupational therapy, or drug and alcohol services as needed. It’s more efficient for the organisation, more beneficial for the person, and more impactful with respect to our mission,” said Reynolds.
“It is a collaborative project, co-led by Clinical Informaticians, IT specialists, and subject matter experts to establish a new standard in connected, patient-centred care,” added Dr. MacKinlay.
“It is a collaborative project, co-led by Clinical Informaticians, IT specialists, and subject matter experts to establish a new standard in connected, patient-centred care.”
Here’s the impact that can come from Barwon’s strategy.
Establishing a new standard indeed; this sort of approach to system design gives organisations like Barwon a foundation that:
- Empowers patients and clinicians
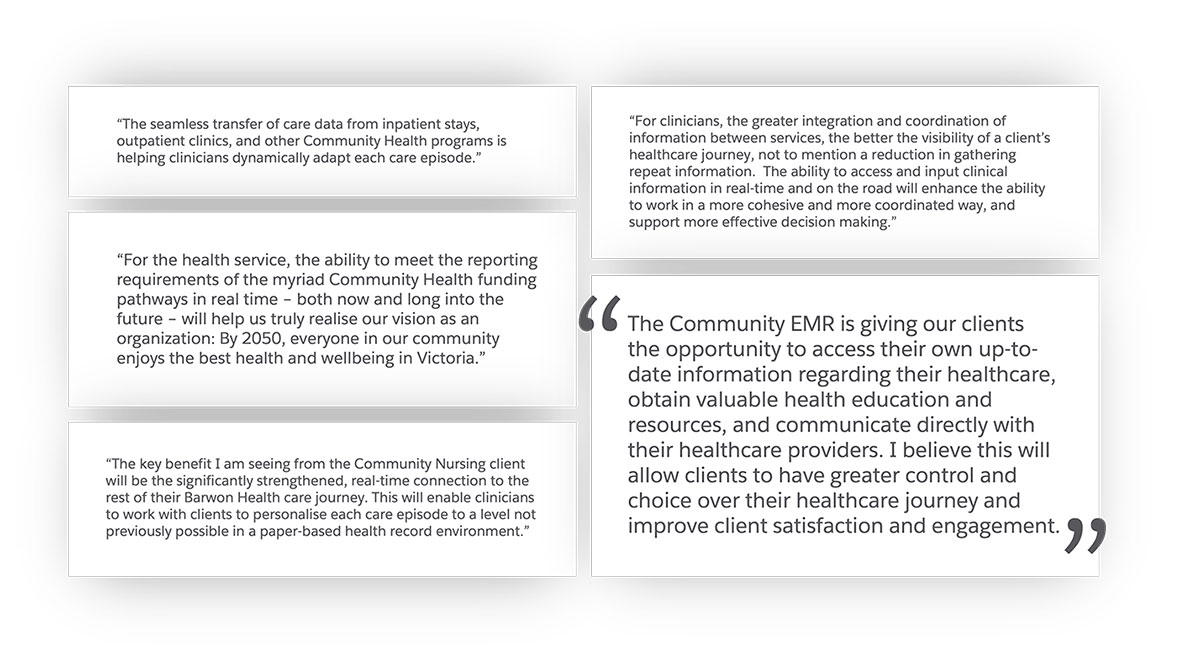
By giving patients the opportunity to take an active role in their care, Barwon is opening up the potential for people to develop a more vested interest in the outcome, “instead of having something done unto them,” said Dr. Jonathan Claydon, (Acting) Medical Informatics Lead, and one of the Barwon Health’s physicians using this system as he works to deliver patient care.
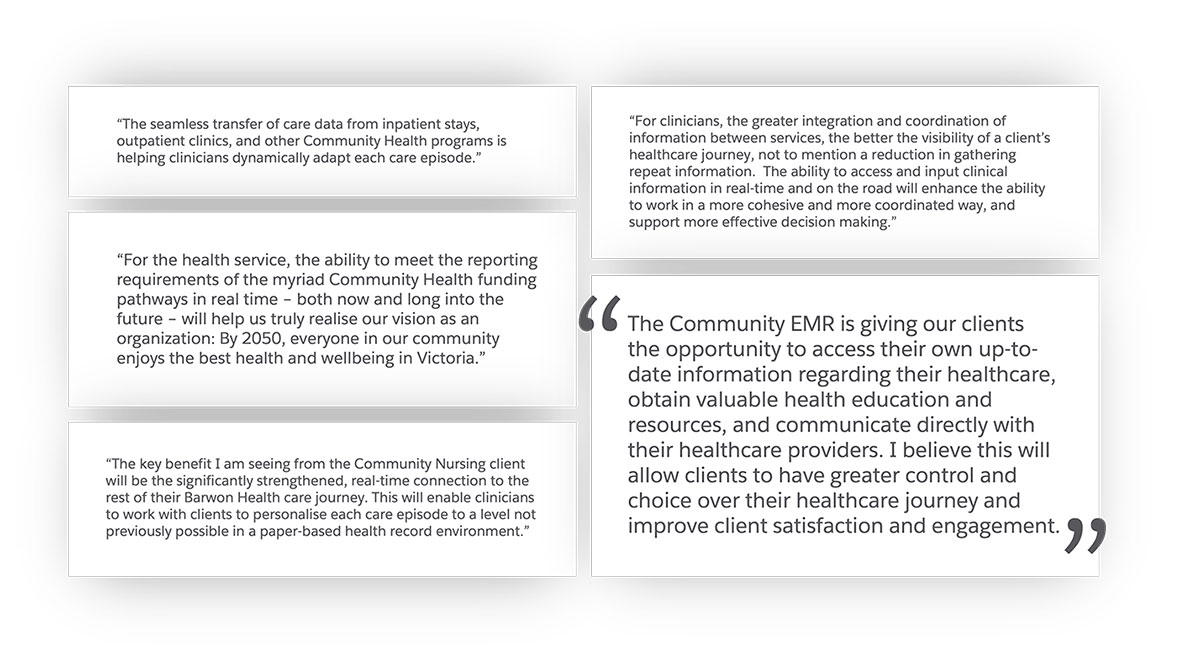
And Dr. Claydon is not the only one who is starting to see the potential of this strategy. Barwon Health’s subject matter experts in Mental Health and Community Nursing have shared the following:
By giving staff 360-degree data visibility, Barwon is giving them the ability to go deeper, see what’s most relevant to their line of work in context, ask more meaningful questions, and be more responsive (if not proactive) with treatment recommendations. The result: higher quality care across a connected set of services. “You can't interrogate a paper document without reviewing the paper document. And individually reviewing 500 paper documents for compliance or for general happiness with a product is impossible,” Dr. Claydon continued.
- Refocuses time and energy on patient care
Storing information in the cloud instead of large data warehouses reduced the amount of IT infrastructure Barwon has to patch and manage. And, “all these individual legacy software options didn't talk to each other, and required repeated data entry,” said Reynolds. “Significant parts of people's days were spent having to retype information filled out on paper forms from legacy systems that did not meet compliance requirements. So, data and reporting have been a big deal for us as that was a real pain point for clinicians.” Think about the impact that could come from applying that time and budget to areas like patient care, research, equipment improvements, etc.
- Reinforces trust imperatives
Integrated billing functions, next on Barwon’s to-do list, will not only reduce the same clerical work that might otherwise chip away at focus and productivity but can also mitigate errors data entry errors or gaps in service due to fragmented information.
Integrated reports and dashboards mean people can click a link, log in, and find the data they need in real-time instead of having to, say, download a spreadsheet attached to an email — something that is difficult to track who it’s been shared with, if that was shared across a secure environment, or to rely upon as up-to-date information since such documents age with each passing moment.
These impacts are in addition to the basics; this approach will still enable Barwon to measure the metrics and KPIs they’re required to report on, like hospital readmissions, compliance with clinic appointments, compliance with medication, attendance and attrition rates, and more.
“As technology becomes integrated with all aspects of our life, healthcare should be no different. Healthcare doesn’t have to be any more technologically complex,” said Dr. MacKinlay. “Utilising the cloud and optimising that for a more patient-centric approach allows us to have the same level of safe and comfortable interaction with the technology that is seen in any other industry.”
Keep exploring stories like this one.
Questions? We’ll put you on the right path.
Ask about Salesforce products, pricing, implementation, or anything else — our highly trained reps are standing by, ready to help.